Abstract
Introduction Universal allogeneic donor CAR T cells are being developed as part of a 'deep conditioning' strategy against AML to secure disease clearance ahead of allogeneic stem cell transplantation (Allo-SCT). CD33 is widely expressed on AML, sometimes on the entire leukemia-associated populations, but is also present on healthy precursors; CD7 may be expressed on AML subpopulations and is present on normal T and NK cells, resulting in problematic fratricide effects during CAR T manufacture. Healthy donor derived CAR T cell banks generated using cytidine deamination base-editing and lentiviral transduction with CARs against both CD33 and CD7 circumvent such issues and could offer cell based anti-leukemic therapy alongside preparative effects ahead of allo-SCT. Here we investigated single and combinational BE-CAR T cells against primary human AML in vivo.
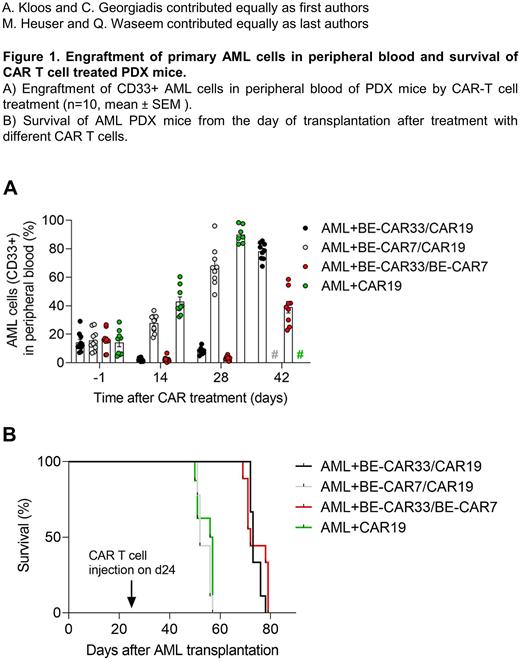
Methods: Healthy donor lymphocytes were activated by anti-CD3/28 stimulation ahead of electroporation to deliver codon optimised base editor mRNA and guide RNAs against CD7, CD52 and TRBC, and lentiviral transduction to express either an anti-CD7 or anti-CD33 CAR. Magnetic bead depletion removed residual TCRab T cells, and disruption of CD7 ensured cells avoided fratricide. In vitro, antigen specific function was verified in cytotoxicity and cytokine release assays, and in vivo potency was confirmed against luciferase modified Molm14 and Kasumi lines in NSG mice. Responses against primary AML were investigated in a patient derived xenograft model (PDX) from a KIT mutated AML patient, established by serial transplantation, with full expression of CD33 (100% of blasts) and partial expression of CD7 (30% of blasts). Cells were injected into irradiated NSG mice (n=10 per group). On day 24 at a mean leukemic engraftment of 15% human CD45 positive cells in peripheral blood, mice were treated with either 10x106 BE-CAR33, BE-CAR7 or a combination of both or with anti-CD19-CAR-T cells (CAR19) as a control group (in total 20x106 T cells per mouse). AML engraftment, T cell persistence and expression of checkpoint markers were monitored by multicolour flow cytometric analysis.
Results: On days 14 and 28 after CAR-T cell infusion, AML cells were readily detected in peripheral blood of control CAR19 animals (42.8% and 90% respectively) and the BE-CAR7 group (27.8% and 67.6%), but were notably reduced in the BE-CAR33 alone group (2.3% and 8.3%) and the BE-CAR33 and BE-CAR7 combination group (2.5% and 3.4%) (Figure 1A). Survival was significantly prolonged for BE-CAR33 and BE-CAR33/BE-CAR7 treated mice compared to the other groups (P<0.001) (Figure 1B). CD7+ AML cells were depleted to a mean of 1% and 4.5% in the BE-CAR33 group, to 0.6% and 0.7% in the BE-CAR33/BE-CAR7 and to 2.6% and 2.9% in the BE-CAR7 group, while CD7+ AML cells increased to 12% and 30% in the CAR19 group at day 14 and 28 after CAR-T cell infusion. Total CD2+CAR-T cell detection in peripheral blood ranged from 1.6 to 9.8% at day 14, 1 to 3.7% at day 28, and 0.8 to 2.7% at day 42, indicating durable persistence over the investigation period. Interestingly, PD-L1 on AML cells was present in all groups while checkpoint markers PD1, GAL9, TIM3, and LAG3 were significantly upregulated in BE-CAR33 cell treated mice, but not BE-CAR7 or CAR19 cell treated mice (P<0.001 for all comparisons).
Conclusions: Lentiviral transduction and multiplexed base editing to remove TCR, CD52 and the shared AML/T lineage antigen CD7, enabled the generation of universal donor CAR T cells for combinational use. This data demonstrates robust activity of BE-CAR33 alone and in combination with BE-CAR7 against human CD7+CD33+AML in mice and highlights the importance of strategies that ensure complete targeting of leukemic populations.
Disclosures
Heuser:Abbvie: Consultancy, Honoraria, Research Funding; Eurocept: Honoraria; Jazz Pharmaceuticals: Consultancy, Honoraria, Research Funding; Janssen: Honoraria; Novartis: Consultancy, Honoraria, Research Funding; Takeda: Honoraria; Agios: Consultancy, Research Funding; BMS: Consultancy; Daiichi Sankyo: Consultancy, Research Funding; Glycostem: Consultancy, Research Funding; Kura Oncology: Consultancy; Pfizer: Consultancy, Research Funding; PinotBio: Consultancy, Research Funding; Roche: Consultancy, Research Funding; Tolremo: Consultancy; Astellas: Research Funding; Bayer Pharma AG: Research Funding; BergenBio: Research Funding; Loxo Oncology: Research Funding. Qasim:Kite & Virocell: Consultancy; Tessa Therapeutics: Consultancy; Novartis: Consultancy; Wugen: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal